As an intuitive and inductive thinker, I often use facts to prove or disprove my biases. This may make me a poor researcher, though I believe I would have been popular in circa 1200 academic circles. Serendipity plays a role; yes I’m a big Nassim Taleb fan – sometimes in the seeking, unexpected answers appear. Luckily, I’m correct more often than not. But honestly – in predicting widely you miss more widely.
One of my early mentors from Wall St. addressed this with me in the infancy of my career – take Babe Ruth’s batting average of .342 . This meant that two out of three times at bat, Babe Ruth struck out. However, he was trying to hit home runs. There is a big difference between being a base hit player and a home run hitter. What stakes are you playing for?
With that said, this Blog is for exploring topics I find of interest pertaining mostly to healthcare and technology. The blog has been less active lately, not only due to my own busy personal life (!) but also because I have sought more up-to-date information about advancing trends in both the healthcare payment sector and the IT/Tech sector as it applies to medicine. I’m also diving deeper into Radiology and Imaging. As I’ve gone through my data science growth phase, I’ll probably blog less on that topic except as it pertains to machine learning.
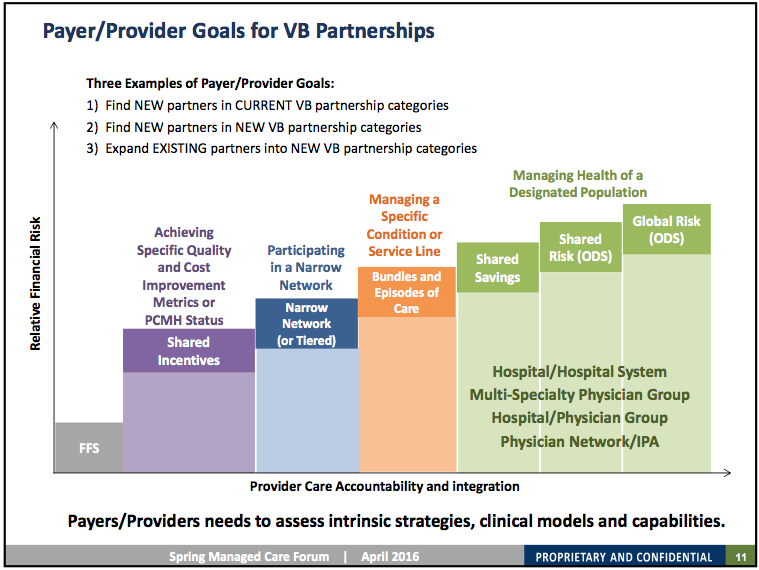
The evolution of the volume to value transition is ongoing as many providers are beginning to be subject to at least a degree of ‘at-risk’ payment. Stages of ‘at-risk’ payment have been well characterized – this slide by Jacque Sokolov MD at SSB solutions is representative:
In 2015, approximately 20% of medicare spend was value-based, with CMS’s goal 50% by 2020. Currently providers are ‘testing the waters’ with <20% of providers accepting over 40% risk-based payments (c.f. Kimberly White MBA, Numerof & Associates). Obviously the more successful of these will be larger, more data-rich and data-utilizing providers.
However, all is not well in the value-based-payment world. In fact, this year United Health Care announced it is pulling its insurance products out of most of the ACA exchange marketplaces. While UHC products were a small share of the exchanges, it sends a powerful message when a major insurer declines to participate. Recall most ACO’s (~75%) did not produce cost savings in 2014, although more recent data was more encouraging (c.f. Sokolov). Notably, out of the 32 Pioneer ACO’s that started, only 9 are left (30%) (ref. CMS). The road to value is not a certain path at all.
So, with these things in mind, how do we negotiate the waters? Specifically, as radiologists, how do we manage the shift from volume to value, and what does it mean for us? How is value defined for Radiology? What is it not? Value is NOT what most people think it is. I define value as: the cost savings arising from the assumption and management of risk. We’ll explore this in my next post.